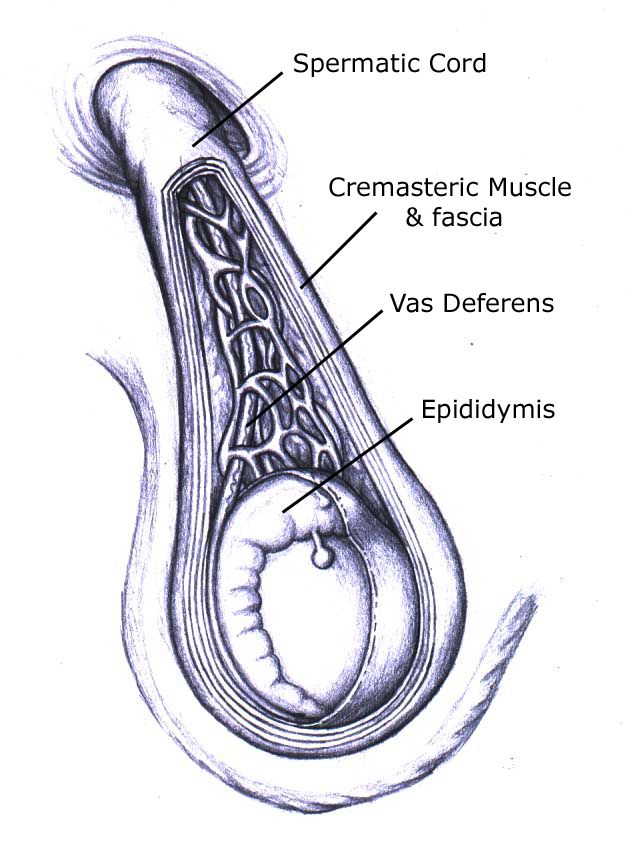
The spermatic cord, despite its name, is not one structure but a collection of structures that pass through the deep inguinal ring and the fascial coverings contributed by the layers of the abdominal wall. The function of the spermatic cord is to suspend the testis in the scrotum as well as contain structures running to and from the testis.
Where is the spermatic cord located?
The spermatic cord begins at the deep inguinal ring, lateral to the inferior epigastric vessels. It passes through the inguinal canal and exits at the superficial inguinal ring before ending in the scrotum at the posterior border of the testis.
What makes up the outer covering of the spermatic cord?
- Tunica vaginalis. This covers the anterior surface of the spermatic cord just above the testis.
- Internal spermatic fascia. Made up of the transversalis/endoabdominal fascia.
- Cremasteric fascia. Made up of the fascia of the internal oblique muscle. This also contains the cremasteric muscles which draw the testis superiorly into the scrotum when it is cold and lower the testis away from the body when it is warm.
- External spermatic fascia. Composed of the aponeurosis of the external oblique muscle.
What does the spermatic cord contain?
Spermatic Structures
These transport sperm from the testis during ejaculation.
- Ductus deferens. Vas deferens conveys sperm from the epididymis to the ejaculatory duct.
Arteries
These bring oxygen-rich blood to the testis
- Testicular artery. This is the main vessel supplying blood to the testis and arises from the abdominal aorta at L2.
- Artery of the ductus deferens. Arises from inferior vesical artery.
- Cremasteric artery. This is the major vessel supplying blood to the cremasteric muscle and arises from the inferior epigastric artery.
Veins
These take used, oxygen-poor blood back to the heart.
- Pampiniform plexus. This structure is formed by up to 12 veins and drains into the right and left testicular veins.
Nerves
These convey instructions between the brain and the testis.
- Sympathetic nerve fibers on arteries
- Sympathetic and parasympathetic nerve fibers on the ductus deferens
- Genital branch of the genitofemoral nerve supplying the cremaster muscle
Lymphatics
These structures monitor body fluid for infection and help fight them when they occur.
- Lymphatic vessels draining the testis and closely associated genital structures
- Lumbar lymph nodes draining the remainder of the pelvic structures
Spermatic cord and vasectomy
Some men may be understandably concerned that their testicles will hang or move differently following a vasectomy procedure. Many diagrams and illustrations on the internet would appear to suggest that the vas deferens is the only thing attaching the testis to the body. In reality, the vas deferens is just one small part of the larger group of structures making up the spermatic cord, and the remainder of these other structures are not damaged or cut during a vasectomy.
Testosterone made in the testicles is circulated throughout the rest of the body by way of the veins and arteries in the spermatic cord. These vessels are not damaged during a vasectomy, which is why testosterone levels in the body are not affected by the vasectomy procedure. These blood vessels together with a multitude of nerves, muscles, and lymphatic structures support the weight of the testicles in the scrotum. The vas deferens, which is a thin, stiff tube running through the middle of the spermatic cord, delivers sperm made in the testis and is the only thing cut during the procedure.
One challenge doctors face before a vasectomy is separating the tubes of the vas deferens from the rest of the structures in the cord. They usually do this at a pre-vasectomy consult (the “tube check”), where they confirm that the tubes of your vas deferens are easy to locate and that there is no suggestion of any special problems. This “tube check” is performed a second time during the vasectomy itself before any cuts are ever made.
Suggested readingSummary
The spermatic cord is a cord-like structure in the male reproductive system. It’s located in the groin and scrotum and it contains as well as arteries, veins, cremasteric muscles, nerves, and lymphatic vessels. The spermatic cord performs several physiologic functions and connects the testicles to the rest of the body.
During a vasectomy, the spermatic cord is not severed. Only the vas deferens on each testicle is cut.
References and further reading
Vasectomy-Information.com has a strict sourcing policy. We rely on evidence-based medicine, peer-reviewed studies, reputable clinical journals, and medical associations. Learn more about how we ensure our content is accurate and up-to-date by reading our editorial policy.- Galejs L. Diagnosis and treatment of the acute scrotum. Am Fam Physician. 1999;59(4):817-824. https://www.aafp.org/afp/1999/0215/p817.html
- Sam W. Spermatic cord (anatomy). YouTube. Published April 4, 2018. https://www.youtube.com/watch?v=v9eNKf3MJAo
- Spermatic cord. IMAIOS. https://www.imaios.com/en/e-Anatomy/Anatomical-Parts/Spermatic-cord
- The Spermatic Cord – Course – Fascia – Contents. TeachMeAnatomy. Published April 5, 2020. https://teachmeanatomy.info/pelvis/the-male-reproductive-system/spermatic-cord/