There are numerous points to be considered by men, women, or couples when deciding which method of birth control is right for them. The effectiveness and reliability of the procedure are on top of that list. A vasectomy is one of the most effective birth control options available, and the most effective method for men. However, no medical procedure is 100 percent foolproof. Vasectomy failure is rare, but it can happen.
What are the chances a vasectomy will fail?
It’s reported pregnancy occurs only in 1 to 2 out of every 1000 couples in which the man has had a vasectomy.1 However, it’s important to note that most vasectomy failures happen soon after the procedure. Vasectomies don’t make men sterile overnight. The procedure stops the flow of new sperm cells into the semen. The semen that has already made it past the spot where the tube is cut can still produce a pregnancy. Doctors check their patient’s semen after the procedure to make sure it is infertile. Until then, couples must use other means of contraception.
Both the American Urological Association (AUA) and the Royal College of Obstetricians & Gynaecologists (RCOG) give vasectomy a 0.05 percent (1 in 2000) chance of failure.23 This figure is based on men who were given clearance after a semen sample. One study puts the rate at 0.025 percent (1 in 4000) when DNA-proven paternity of post-vasectomy babies was taken into account.4
Some men still have healthy semen for a long time after their procedure. Most of these men will become infertile within 6 months. However, a small percentage of men remain fertile after six months, when the leftover sperm cells from before their surgery should all be dead and gone. In this case, something called recanalization has happened. Recanalization is the spontaneous re-joining of the cut ends of the vas deferens.
Because healthy sperm can find their way back into the semen, there are two types of vasectomy failures.
- Technical failures. If semen still contains healthy sperm cells six months after a vasectomy, the procedure is considered a technical failure. As we have just said, the most common reason for technical failure is recanalization. Another, less common, reason for technical failure is an error on the part of the surgeon doing the procedure. In both cases, the vasectomy must be redone. According to the AUA, the technical failure rate for a vasectomy is between zero and one percent.2
- Contraceptive Failures. When someone does become pregnant and the father has had a vasectomy, it’s called a contraceptive failure. For this to happen, the sperm has to find its way back into the semen long after the procedure. Because there is no testing to warn anybody, this is when a post-vasectomy pregnancy occurs. This is, thankfully, very rare.
Recommended product
Home Vasectomy Test Kit
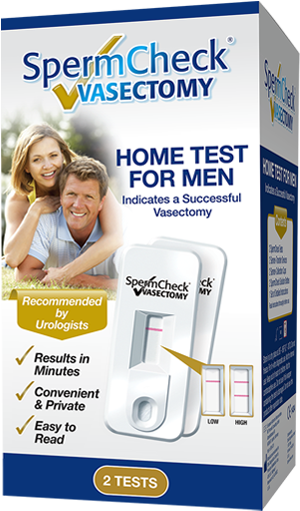 View on Amazon Read our review We only recommend products we think are useful for our readers. If you make a purchase, we may earn a small commission.
View on Amazon Read our review We only recommend products we think are useful for our readers. If you make a purchase, we may earn a small commission.How does vasectomy compare to other methods of birth control?
The table below compares the failure rates for different birth control methods and is based on a study that conducted a comprehensive review of the literature on contraceptive failure. It should be noted that the review arbitrarily set the typical- and perfect-use estimates for vasectomy.
| Method | Perfect use | Typical use |
|---|---|---|
| Vasectomy (Male sterilization) | 0.10% | 0.15% |
| Implant (Nexplanon) | 0.05% | 0.05% |
| LNG IUD (Levonorgestrel intrauterine system) | 0.2% | 0.2% |
| Tubal ligation (Female sterilization) | 0.5% | 0.5% |
| IUD (Copper T intrauterine device) | 0.6% | 0.8% |
| Injection or “shot” (Depo-Provera) | 0.2% | 6% |
| Vaginal ring (NuvaRing) | 0.3% | 9% |
| Patch (Evra) | 0.3% | 9% |
| Pill (Combined pill and progestin-only pill) | 0.3% | 9% |
| Diaphragm | 6% | 12% |
| Condom (Male) | 2% | 18% |
| Internal condom (Female) | 5% | 21% |
| Withdrawal (Pull out method) | 4% | 22% |
| Fertility awareness methods (FAMs) | 3-5% | 24% |
| Spermicides | 18% | 28% |
Can a vasectomy reverse itself?
An unintended post-vasectomy reversal is known as recanalization. Recanalization is a process in which sperm regains the ability to enter a man’s semen after a vasectomy, resulting in the remote possibility of pregnancy.
Suggested readingHarvard Medical School reports that recanalization occurs in approximately 1 in 4000 vasectomies.5 Other studies have indicated that about 1 out of 2000-3000 men will experience a late failure.6 So this figure will vary from source to source, but the bottom line is that recanalization is a very rare phenomenon.
Even when recanalization does occur, the resulting sperm counts are typically much lower than before and are less likely to result in a pregnancy. Just because a man has had a recanalization doesn’t mean he will have pre-vasectomy levels of fertility.
How does recanalization happen?
Recanalization is a process where a lot of unlikely things have to happen at the same time:
- Sperm cells have to leak out of the closed vas.
- New smaller tubes have to form around groups of the “floating” sperm cells.
- One of the newly formed tubes has to make it to the other cut end.
How is recanalization detected?
When it happens early after the procedure, then sperm cells will stubbornly remain in the semen. Doctors check the semen during the post-vasectomy semen analysis to make sure the old sperm cells have all died out and will recognize early recanalization before anyone becomes pregnant. Sperm cells don’t live forever. So, when there is still healthy sperm in the semen six months after surgery we know that it isn’t because the old sperm have stuck around. That is how doctors can know an early recanalization has happened. A doctor will then redo the surgery, taking extra care to put additional layers of tissue between the separated ends of the vas.
Sometimes recanalization does not happen until years after the initial surgery. This event is called “late recanalization” or “delayed recanalization.” In the case of late recanalization, the semen will have looked sperm-free on earlier testing. The doctor will have given their patient an all-clear.
So, in these delayed cases, how would someone even know the sperm found its way back into the semen? Well, we usually find out when the female partner (a long time later) becomes pregnant. The urologist will ask to take another look at the semen, and there will be sperm again. Miracle baby! All kidding aside, this has happened before. It happens about once out of every two thousand times the procedure is done. In case you missed it, late recanalization is the cause of contraceptive failure.7
Summary
The chances of a woman becoming pregnant after her partner has had a vasectomy are incredibly slim. There are very few guarantees in medicine. Some treatments come close to 100% effectiveness, but very few achieve this goal. The vasectomy procedure is one of the treatments that come pretty close.
As far as other forms of birth control, most of them are not permanent and require some maintenance or rule-following. Because of that, most other forms of birth methods are subject to human error, which lowers their effectiveness.
Failure rates and effectiveness are important considerations for the choice of contraception but there are other considerations like cost, the risks of complications, and the irreversibility of the procedure.
References and futher reading
Vasectomy-Information.com has a strict sourcing policy. We rely on evidence-based medicine, peer-reviewed studies, reputable clinical journals, and medical associations. Learn more about how we ensure our content is accurate and up-to-date by reading our editorial policy.- Trussell J. Contraceptive failure in the United States. Contraception. May 2011:397-404. doi:10.1016/j.contraception.2011.01.021
- Sharlip ID, Belker AM, Honig S, et al. Vasectomy: AUA guideline. J Urol. 2012;188(6 Suppl):2482-2491. doi:10.1016/j.juro.2012.09.080
- Sterilisation for women and men: what you need to know. Royal College of Obstetricians and Gynaecologists (RCOG) https://web.archive.org/web/20110104225418/http://www.rcog.org.uk/womens-health/clinical-guidance/sterilisation-women-and-men-what-you-need-know#how. Archived from the original.
- Sterilisation (vasectomy and tubal occlusion) – Contraception. Sexwise, Family Planning Association (FPA) https://www.sexwise.fpa.org.uk/contraception/sterilisation
- Barry R. Male contraception and no-scalpel vasectomy. BCMJ. 2001;43(10):560-566. https://www.bcmj.org/articles/male-contraception-and-no-scalpel-vasectomy
- Vasectomy and Vasovasostomy (Reversal Surgery). Well-Connected reports. Harvard Medical School. September 2001.
- Labrecque M, Hays M, Chen-Mok M, Barone MA, Sokal D. Frequency and patterns of early recanalization after vasectomy. BMC Urol. September 2006. doi:10.1186/1471-2490-6-25